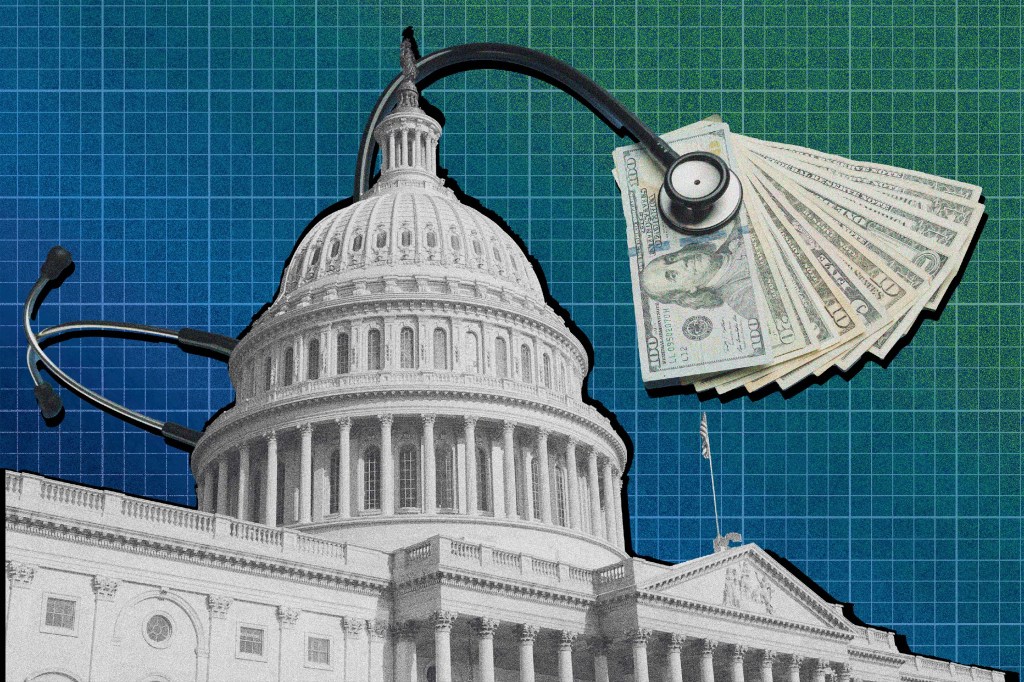
It seems simple: Require hospitals and insurers to post their negotiated prices for most health care services and — bingo — competition follows, yielding lower costs for consumers.
But nearly four years after the first Trump administration’s regulations forced hospitals to post massive amounts of pricing information online, the effect on patients’ costs is unclear. And while President Joe Biden added requirements to make pricing information more user-friendly, Donald Trump’s imminent return to the White House has raised questions about what’s next, even though posting prices is an area of rare bipartisan agreement.
The uncertainty of what might happen next led some proponents to lobby Congress to include hospital and insurer price transparency in must-pass legislation before Trump takes office. That would turn both his and Biden’s regulations into law, making them less susceptible to being weakened or repealed by a future administration. But that effort failed.
The legislative step could also help protect against legal challenges in the wake of a Supreme Court decision that limited government agencies’ regulatory authority.
Employers are using transparency data to try to slow growth of their health care costs, and “the last thing you want to do is start over,” said James Gelfand, president and CEO of the ERISA Industry Committee, which represents large employers who finance their own health plans. His group is among the organizations pressing Congress to act.
“Congress’ failure to act is deeply disappointing, but employers and other advocates will redouble our efforts,” Gelfand said. “This will get done.”
While there are reports that many hospitals are not fully complying, federal regulators have sent thousands of warning letters to hospitals and fined just over a dozen.
Email Sign-Up
Subscribe to KFF Health News’ free Morning Briefing.
The transparency rules require hospitals to list the prices they accept from all insurers for thousands of items and services, from stitches to delivery room costs to X-rays. For consumers, hospitals must also provide a list of 300 “shoppable” services, including bundled prices accepted for common services such as having a baby or getting a hip replacement. Insurers in July 2022 were similarly required to list their negotiated prices, not only for care at hospitals, but also surgery centers, imaging facilities, laboratories, and doctors’ offices.
It’s a massive and often confusing amount of data that has drawn interest from researchers and commercial outlets like Turquoise Health, which has sought to organize the information to better help ordinary consumers shopping for medical services or employers overseeing workers’ health plans.
The data shows a huge variation in prices, both in what hospitals charge and what insurers pay, for the same services. But the result of making those prices public is so far hard to quantify.
A recent study by Turquoise looked at negotiated rates in the nation’s 10 largest metro areas for a set of common health care services. It found that rates in the top quarter tier — the most expensive category — declined by 6.3% from December 2021 to June 2024, during the time the transparency rules were in place. But negotiated rates for the lowest-cost tier of services rose by 3.4%.
That may indicate hospitals and insurers — who can now see what rivals are charging and paying — have either cut prices or demanded better rates, at least for the costliest services.
Even so, Gerard Anderson, who oversees research into the data as a professor at the Bloomberg School of Public Health at Johns Hopkins University, said the changes Turquoise noted were small and are not reflective of what his team has seen in their own studies.
“So far we have not detected any impact of this data on behavior, of where insurers decide to go or what hospitals do to change prices once they realize what others are charging,” Anderson said.
Some health policy experts think it’s unlikely the incoming Trump administration would reverse its prior commitment to price transparency.
“I don’t see a world where he tanks his own regulations,” said Joe Wisniewski, an associate vice president at Turquoise Health. “There is also so much broad bipartisan support on the Hill.”
The current price-posting rules began with requirements in the Affordable Care Act, which the initial Trump administration more fully defined. The hospital industry failed in a legal challenge to block those rules, and the Trump-era requirements became effective in January 2021.
But even after the Biden administration made the data more user-friendly, it’s still not very helpful to consumers, Anderson said.
“This data is not telling them the price they will pay. It’s telling them the average price people paid last month or last quarter for a similar type of service,” he said.
More useful, Anderson and other experts say, are requirements in the price transparency rules that demand insurers offer online calculators for hundreds of nonemergency services. The detailed cost estimates must take into account how much patients have paid toward annual deductibles.
For uninsured consumers or others who don’t have access to online calculators, it remains difficult to piece together how much a service might cost from the information hospitals post online. For one thing, not every hospital has posted its negotiated rates.
The Department of Health and Human Services’ inspector general said in November an audit of 100 hospitals found that 63 complied with the price transparency rule, while the rest failed to meet one or more requirements.
The advocacy group Patient Rights Advocate, which looked at a sample of 2,000 hospitals, says that only 21% were fully compliant, although it used broader measures for compliance than the inspector general.
“By keeping their prices hidden, hospitals continue to block American consumers from their right to compare prices and protect themselves from overcharges,” said Cynthia Fisher, founder and chairman of the group, which has called for stricter rules and enforcement.